Working remotely from scenic countryside locations or small mountain towns might seem like the perfect digital nomad dream, but accessing quality medical care in these picturesque settings presents unique challenges. Healthcare in rural areas often involves longer distances to medical facilities, fewer specialized services, and limited emergency response capabilities that urban nomads take for granted. Understanding these realities before settling into rural destinations can make the difference between a seamless remote work experience and a medical emergency that derails your nomadic plans.
The transformation of remote work has led many digital nomads to seek destinations beyond crowded cities, drawn to rural areas offering lower costs, natural beauty, and authentic cultural experiences. However, healthcare in rural areas requires strategic planning, comprehensive insurance coverage, and awareness of local medical resources to ensure your health and safety while maintaining your location-independent lifestyle. This comprehensive guide explores the challenges and solutions for accessing quality healthcare in rural areas as a digital nomad.
Understanding the rural healthcare landscape
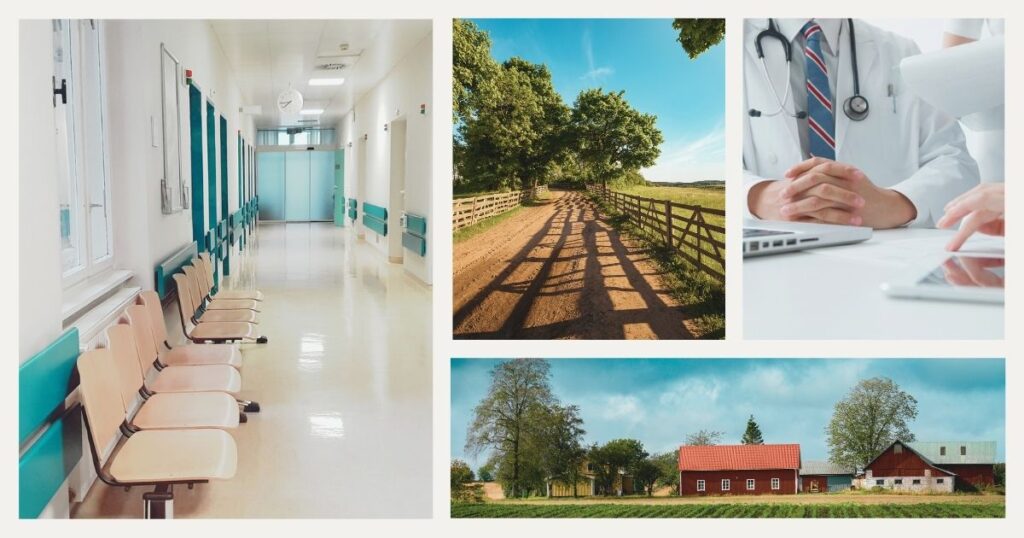
Healthcare in rural areas operates under fundamentally different constraints than urban medical systems, creating both challenges and opportunities for digital nomads who choose to work from remote locations. Rural healthcare systems typically serve smaller populations across larger geographic areas, resulting in resource allocation challenges that affect medical service quality and availability.
Geographic and infrastructure barriers
Distance represents the most immediate challenge, with patients often traveling hours to reach specialized facilities or emergency services. Rural hospitals may be 50-100 miles apart, and emergency response times can be significantly longer than in urban areas, where ambulances arrive within minutes.
Infrastructure limitations compound geographic challenges. Rural areas often have limited internet connectivity, affecting telemedicine capabilities, while poor road conditions, seasonal weather challenges, and limited transportation options make accessing healthcare in rural areas even more difficult during emergencies or routine care.
💡 Did you know? Rural areas in the United States have lost over 180 rural hospitals since 2005, creating larger gaps in healthcare access and forcing patients to travel greater distances for basic medical services.
Provider shortages and specialization gaps
Healthcare in rural areas typically suffers from physician shortages, with rural areas having significantly fewer doctors per capita than urban regions. This shortage is particularly acute for specialized medical services, with many rural areas lacking specialists in cardiology, oncology, or other critical medical fields.
The physicians practicing in rural areas often serve as generalists, handling a broader range of medical conditions than their urban counterparts who can specialize more narrowly. While this provides comprehensive primary care, it may mean referrals to distant specialists for complex conditions.
Mental health services are particularly scarce in rural healthcare systems, with many areas having no psychiatrists or licensed mental health counselors within reasonable traveling distance. This gap can be especially challenging for digital nomads dealing with isolation or work-related stress.
Despite infrastructure challenges, technology is revolutionizing healthcare in rural areas through telemedicine and remote monitoring capabilities. High-speed internet enables video consultations with specialists located hundreds of miles away, bringing expert medical care to remote locations.
🌟 Pro tip: ensure reliable internet connectivity for accessing telemedicine services with a dependable rural connectivity solution that provides consistent coverage even in remote areas where traditional mobile networks may be weak or unreliable.
Digital nomad-specific rural healthcare challenges
Digital nomads face unique healthcare challenges in rural areas that differ from those experienced by permanent rural residents. These challenges stem from unfamiliarity with local healthcare systems, lack of established patient relationships, and temporary stays in rural locations.
Establishing care without local connections
Unlike permanent residents who develop relationships with local healthcare providers over time, digital nomads must quickly identify and access healthcare in rural areas without established connections. This can be particularly challenging in rural communities where healthcare providers may prioritize established patients or have limited capacity for new patients.
Rural healthcare providers may be unfamiliar with the unique needs of digital nomads, including flexible appointment scheduling, travel health advice, or coordination of care across multiple locations. Understanding how to communicate your nomadic lifestyle while establishing credibility with rural healthcare providers becomes essential for accessing quality care.
Insurance networks and coverage areas add complexity, as digital nomads may find their health insurance plans have limited provider networks in rural areas, potentially resulting in higher out-of-pocket costs or the need to travel to network providers in distant locations.
Emergency preparedness and response
Emergency medical situations present heightened risks for digital nomads in rural areas due to longer response times and limited local emergency services. Understanding local emergency protocols, nearest hospital locations, and emergency contact procedures becomes critical for nomads working from remote locations.
Many rural areas have volunteer emergency services with limited resources compared to professional urban emergency services. Digital nomads should research emergency capabilities in their chosen rural locations and plan accordingly for potential medical emergencies.
Communication during emergencies can be challenging in rural areas with poor cell phone coverage or unreliable internet connections. Having multiple communication methods and emergency contact information readily available becomes essential for accessing help when needed.
💡 Did you know? Many rural areas rely on helicopter emergency medical services for serious cases, but weather conditions, time of day, and distance can affect availability, making ground transportation the only option in many emergency situations.
Prescription medication access represents a significant challenge for healthcare in rural areas, with many rural communities served by a single pharmacy or requiring travel to distant towns for medication pickup. Digital nomads with chronic conditions requiring regular medications must plan carefully when choosing rural destinations.
Health insurance and technology solutions for rural healthcare

Navigating health insurance coverage for healthcare in rural areas requires understanding network limitations and coverage gaps. Health insurance networks often have limited representation in rural areas, with fewer in-network providers available, potentially resulting in higher out-of-pocket costs for digital nomads.
Emergency medical evacuation coverage becomes particularly important for healthcare in rural areas, where local facilities may lack the capability to handle serious conditions. This coverage can include ground ambulance transport or helicopter evacuation in critical situations.
Many modern health insurance plans include telemedicine coverage, which can be valuable for accessing healthcare in rural areas. These benefits may include video consultations with specialists, mental health counseling, and routine follow-up appointments that don’t require in-person visits.
🌟 Pro tip: consider supplemental travel insurance that specifically covers adventure activities and remote area evacuation if your primary health insurance has limitations for rural or outdoor activities.
Technology serves as a critical bridge for accessing quality healthcare in rural areas. Telemedicine platforms have revolutionized healthcare access by connecting patients with providers regardless of geographic location, offering video consultations and digital prescription services.
Digital nomads can use telemedicine to maintain continuity with their primary healthcare providers even while working from rural locations. Specialized platforms now offer services designed for remote workers, including occupational health consultations and travel medicine advice.
Wearable health devices and smartphone health apps enable proactive health monitoring while in rural areas where healthcare access may be limited. These technologies can track vital signs, medication compliance, and symptoms that can be shared with healthcare providers during telemedicine consultations.
Final thoughts
Successfully accessing healthcare in rural areas as a digital nomad requires careful planning, appropriate insurance coverage, and leveraging technology to overcome geographic barriers. While rural locations offer unique benefits, including lower costs, natural beauty, and authentic cultural experiences, the healthcare challenges are real and must be addressed proactively to ensure your health and safety while maintaining your nomadic lifestyle.
The key to thriving as a rural digital nomad lies in understanding the limitations of local healthcare systems while maximizing the opportunities provided by modern telemedicine and health technology. By preparing comprehensively, maintaining strong insurance coverage, and staying connected to healthcare resources through technology, digital nomads can successfully work from rural locations while maintaining access to quality healthcare services.
Remember that healthcare in rural areas continues to evolve, with new technologies and service delivery models emerging to address traditional access challenges. Staying informed about these developments and planning flexibly will help ensure your rural nomadic experiences remain both rewarding and safe.
For digital nomads considering rural destinations, comprehensive health insurance planning is essential. Understanding health insurance options for international travel can help you choose coverage that works effectively in rural and remote locations.
Ready to explore rural destinations while maintaining access to quality healthcare? Nomada provides expert guidance to help you plan safe and successful rural nomadic experiences with confidence 🏥
Frequently asked questions about healthcare in rural areas
Satellite communicators like Garmin InReach or SPOT devices can summon emergency services even without cellular coverage. These devices send GPS coordinates to emergency services and are essential safety equipment for digital nomads working in truly remote rural areas. Always inform someone of your location and expected check-in times when working from areas with limited communication capabilities.
Research healthcare facilities before arriving by checking online reviews, hospital quality ratings, and insurance network directories. Local tourism boards, accommodation hosts, and community bulletin boards often provide healthcare provider recommendations. Telemedicine platforms can also connect you with quality providers regardless of your physical location.
Telemedicine is excellent for routine consultations, prescription refills, and non-emergency health concerns, but cannot replace in-person care for physical examinations, diagnostic tests, or emergency situations. Use telemedicine as part of a comprehensive healthcare strategy that includes knowledge of local emergency services and nearby medical facilities.
Rural health risks vary by location but may include tick-borne diseases like Lyme disease, exposure to farm animals, contaminated water sources, or vector-borne illnesses. Consult with a travel medicine specialist before relocating to rural areas, and research specific health risks associated with your chosen destination to determine appropriate vaccinations and preventive measures.
Establish relationships with mail-order pharmacy services that can deliver to your rural location, and maintain adequate supplies of essential medications. Research local pharmacy availability and establish backup plans for prescription emergencies. Some telemedicine platforms can prescribe medications and coordinate with rural pharmacies for pickup or delivery services.